CORONARY ARTERY DISEASE
CORONARY ARTERY DISEASE
Heart is the pump that undertakes the circulation of blood to and from the systemic circulation. The myocardium itself is supplied with oxygenated blood via the coronary arteries. The coronary artery network consists of the left and right coronary arteries. The left coronary artery provides blood flow to the greatest part of the heart muscle. Its first part is called Left Main Artery and after a while it grants two large branches, the (left) anterior descendant artery and the circumflex artery. About 15-30% of people also have a third branch called ramus intermedius artery.
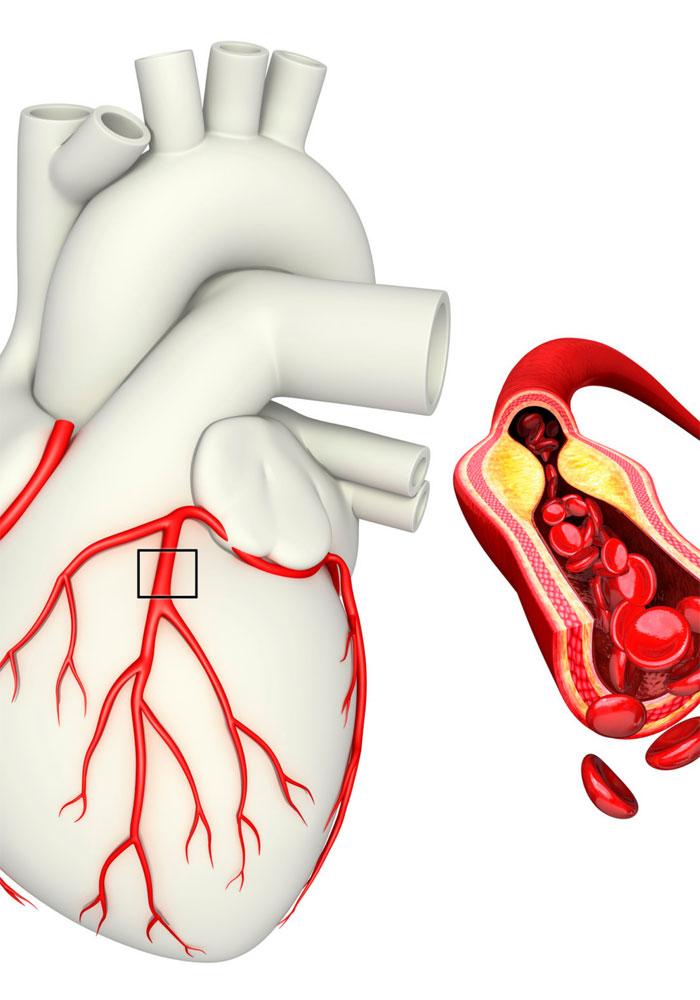
If blood flow through the coronary arteries is not enough to meet the myocardial oxygen needs then this condition is called ischemia. Ischemia may be either caused by reduced blood supply or by increased needs of the myocardium, or by a combination of the two. Reductions in the lumen area of a coronary artery are usually the result of the formation and enlargement of the so-called atherosclerotic plaque.
Coronary artery disease is the development of atherosclerotic plaques on the vessel wall. Predisposing factorsfor coronary aartery disease are: arterial hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, family history of coronary artery disease (manifestation of coronary artery disease in the father under the age of 55 and in the mother under the age of 65) and sedentary way of life.
The process of coronary artery disease is usually gradual and the myocardium adapts to the reduced supply of oxygenated blood. Thus the patient presents with symptoms (chest pain – angina) only when the myocardium requires excessive oxygen supply for some reason, e.g. physical exercise, on the ground of an atherosclerotic plaque that significantly restricts the lumen. This condition was formerly described as stable angina, today it is called chronic coronary syndrome.
“Correction” of a stenosis (called revascularizatoin) in cases of stable angina is conducted with an aim to relief patient symptoms. Still, in cases in which the lesion or combination of lesions puts at risk a large myocardial area, then revascularization is conducted with an expectation to improve prognosis, ie years of life.
Under certain conditions an atherosclerotic plaque can provoke an acute coronary syndrome (unstable angina or acute myocardial infarction). Which exactly are these conditions and which plaques (the vulnerable plaque hypothesis) are the ones that are most prone to cause an acute coronary episode is the subject of long-lasting basic and clinical research. Currently, we accept that plaques with a thin fibrous cap, a large fatty nucleus, intense inflammatory activity and neovascularization are more prone to adverse events.
In the case of acute myocardial infarction in the ruptured (or eroded) atherosclerotic plaque platelets are attracted and attached together with other elements forming a thrombus which partially or completely blocks the blood flow. In this case, revascularization, ie the restoration of blood flow, must be done on an urgent basis and as soon as possible after the start of the episode. If revascularization is timely succeeded, especially within the first 2-3 hours, then the final negative consequences may be negligible for overall heart function. But if there is a delay, then the latter may be significantly affected and the patient may eventually suffer from heart failure.
