AORTIC REGURGITATION
AORTIC REGURGITATION
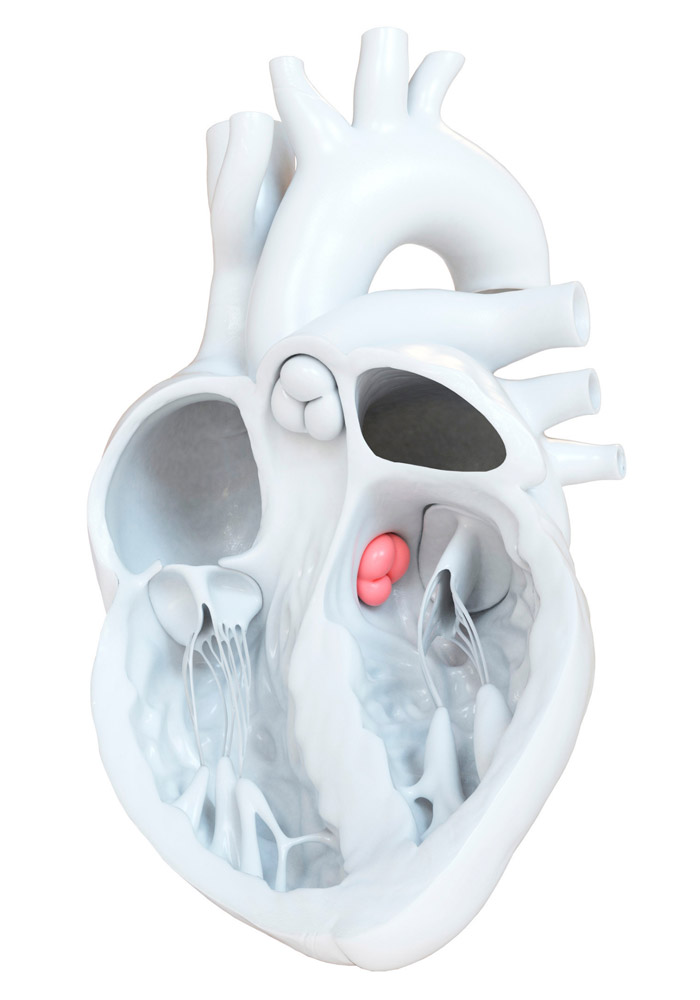
Aortic valve “connects” heart with systematic circulation. In particular it connects left ventricle with the aorta. Aorta is our largest artery which provides with oxygenated blood the human body. Aortic valve “opens” during the systole of the left venticle allowing to the blood to flow forwrard. Subsequently, its cusps close -during left ventricle diastole – not allowing backward flow to blood. Aortic Regurgitatoin (or Aortic Insufficiency) is a condition in which blood flow from the ascending aorta to the left ventricle is present during left ventricular diastole. Physical examinations may reveal clinical signs suggestive of aortc regurgitation (e.g. murmur in heart auscultation, pulse characteristics) but final diagnosis is confirmed via cardiac ultrasonography
Aortic regurgitation in most cases follows a latent clinical course during which heart is able to gradually compensate. Therefore, diagnosis may not be made until first symptoms occur. Left ventricle counterfeits aortic regurgitation by thickening it’s walls maintaing thus a normal systolic function. Gradually, compensations failes to be effective, left ventricle inner dimensions increase, left ventricle ejection fractions is reduced and finally an eccentric remodelling of the ventricle is observed.
Causes
Aortic Regurgiation may be due to a degenerative process or in the context of a bicuspid aortic valve (these two causes represent the two thirds of cases). Aortic regurgitation may also be diagnosed in the context of rheumatic fever history, due to certain drugs (e.g. anorexic), in the context of prosthetic aortic valve (paravalvular leak), trauma, infective endocarditis ή or in the context of aortic syndromes – the last two cases refer to acute aortic regurgitation.
Prognosis
Prognosis of patients suffering from asymptomatic severe aortic regurgitation is estimated to be ~50% 10 years after initial diagnosis; 3 out of 4 will remain asymptomatic for 7 years after initial diagnosis. However, presence of symptoms is related to an adverse prognosis (approximately 2 years; 4 year survival is approximately 30%).
Treatment of Aortic Regurgitation
Chronic severe aortic regurgitation is treated with replacement of the aortic valve, which is -in general- conducted surgically (in selected cases tranascatheter aortic valve implantation may be an option). Prosthetic valve type (bioprosthesis or mechanical) is conducted mainly according to the patients’ age and comorbidities that may require per se chronic anticoagulation.
In the case that diagnosis is made in patient who is already symptomatic, surgical aortic valve replacement should be conducted soon. In contrast, asymptomatic patients will remain in close follow up with the exact intervals being set upon the severity and progression of the case; bi-annually, annually, or even every 3-6 months. The decision to proceed with valve replacement is made when left ventriculat systolic function starts to deteriorate or its dimensions are enlarged in serial echocardiographic evaluation. Indeed, in the case that a patient is to undergo other cardiac surgery (e.g. for coronary artery bypass grafting) valve replacement should be conducted in the same surgical session.
Finally, it is important to underline that acute and chronic aortic regurgitation are two discrete and different entities. Acute aortic regurgitation represents a medical emergency which is potentially lethal and is treated surgically.
