PFO-ASD CLOSURE
TRANSCATHTER PFO-ASD CLOSURE
Closure of an atrial septal defect or open foramen ovale (PFO) can be performed either surgically by a cardiac surgeon or via a transcatheter approach by an invasive cardiologist.
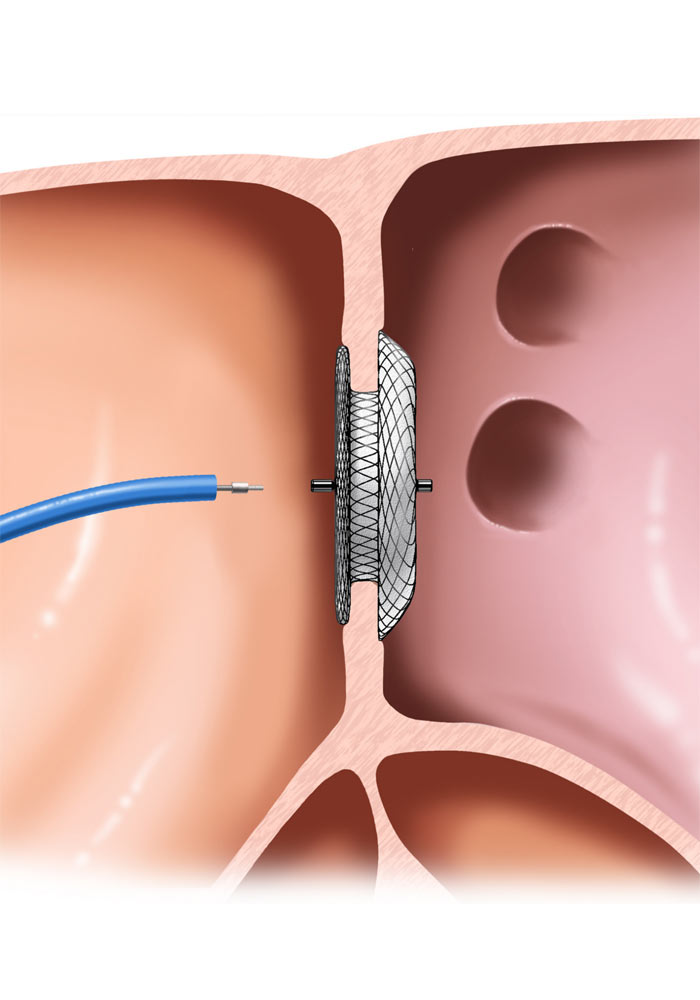
Transcatheter closure is conducted in the catheterization laboratory, which is equipped with an X-ray machine and appropriate infrastructure for vital signs monitoring. The interventional cardiologist punctures the femoral vein – located near the leg – inserts a sheath and via this sheath advances all the necessary “tools” through the venous network to the right atrium. The closure device – usually consisting of two discs – is advanced over special wires and then released in the appropriate position. The procedure is guided by fluoroscopy and echocardiography (esophageal or endocardial). The day after the intervention the patient returns to his daily routine.
Like any invasive procedure, there are risks, but major adverse events are rare. Literature data report closure success rates of ~ 100% (immediate) and 93-96% (fter one year of absolute closure there are). Risks include peripheral venous puncture associated complications, mechanical complications associated with the implantation per se, atrial arrhythmias (0.5 – 15%), immediate or long-term thrombotic complications (1-2%), pericardial effusion or tamponade (0.5 – 1%), embolization of the prosthetic device (0.9-1.3%). The risk for long-term need for cardiac surgery or mortality is reported to be less than 1 in 1000 cases.
