PACEMAKER
PACEMAKER
Mechanical contraction of the heart takes place after electrical stimuli produced by a special area of the heart, called sinus node. Thses stimuli are transmitted in an organized manner first to the atria and then to the ventricles. The great importance of proper functioning of the “electrical” system of the heart is hence easily understood. Any dysfunction may cause symptoms ranging from simple dizziness or temporary loss of consciousness to sudden death. Pacemakers are devices that are implanted to support or completely replace the function of the heart’s electrical system when it is abnormal.
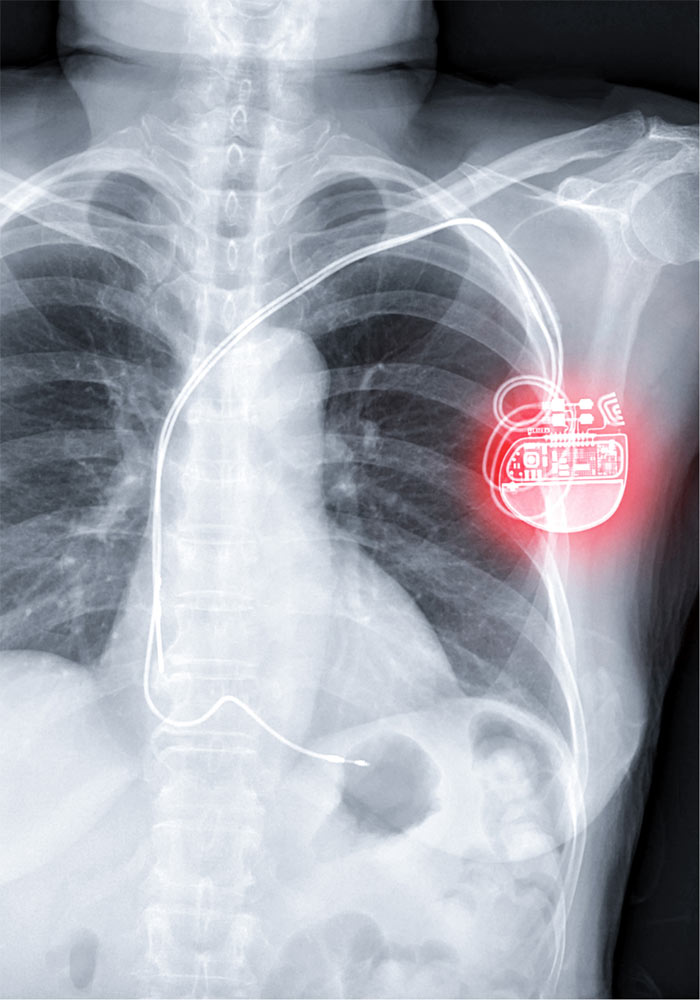
A pacing system consists of the central unit and the “cables” that are placed inside the right heart cavities and are attached to the myocardium. The central unit, called the generator, is about the size of a matchbox, weighs 20-50 grams, and involves the battery, the electronic control unit and special connection ports for the “cables”, which are called electrodes. Depending on the patient’s need for pacing, only a ventricular or both an atrial and a ventricular electrode is placed. The electrodes record real-time electrical activity and the device’s brain decides whether to stimulate or suspend. The purpose of this procedure in to let the native pacing and conduction system function without any intervention, as long as this is feasible.
Procedural Details of Pacemaker Impantation
The implantation of a permanent pacemaker is usually performed under local anesthesia only and / or mild sedation of the patient in a catheterization or electrophysiological laboratory. For implantation, a small incision is made under the clavicle (for the right-handed the left side is preferred) and then venous access is sought. For vascular access, the cephalic vein is usually exposed and if this is not possible, the subclavian vein is punctured. The cardiologist then inserts via the vein access the electrodes and optimizes their position after making some measurements to ensure their proper function. Finally, the physician connects the electrodes to the generator, which then “hides” under the surface of the skin in a special “pocket” – between the skin and the pectoral muscle – which has usually been created just after the initial incision. The operation is completed by the convergence of the skin with suturing or special clips.
After Discharge
The day after the operation the patient is discharged with instructions for the first period after the implantation. During this periord the patient should have somewhat limited mobility of the upper limb on the side the pacemaker was implanted. Additionally, the patient is provided with an “identity card” of the pacemaker which includes the most important data of the device (model, type and number of cables, MRI compatibility). Regarding long-term monitoring, the patient should undergoes annual evaluation of the pacemaker utilizing a special external device (a procedure called interrogation). The interrogation process provides us information about battery life and electrode properties.
Risks
Like any invasive procedure, pacemaker implantation is associated with certain risks which are far less compare to the expected benefit. These risks include mechanical complications during implantation (pericardial effusion, pneumothorax, hemothorax), infections of the “pocket”, the electrodes or the generator. These risks are lower when the jugular vein is selected instead to the vascular access via subclavian and increased the more laborious the implantation of the device. Most complications, if identified early, can usually be treated effectively. In the long run the most important enemy is infections, even in other systems of the body. Thus should be treated promptly and effectively.
LifeSpan – MRI compatibility
More and more pacemaker models are compatible with magnetic resonance imaging (MRI compatible). Modern pacemakers have a lifespan of about 7-8 years. As the end of his life cycle approaches, the treating physician recommends the replacement of the generator. Replacement is a simpler procedure than that of the initial implantation since the electrodes are already in place. A patient with pacemaker should avoid strong magnetic fields (such as in airport’s control) as they are likely to affect its normal function (newer devices are less susceptible to this phenomenon).
Pacemaker without electrodes(Leadless)
The advent of leadless pacemaker systems is a real revolution. These devices are about the length of a small coin. The implantation process is extremely simplified. The device is implanted with special manipulations in the right ventricular myocardium after being advanced there following a puncture of the right or left femoral vein.
Leadless pacemakers, in addition to feautring an easier implantation process, they have the advantage of not needing “cables” so they lack all the possible complications associated with the presence of an additional prosthetic stuctures inside the heart. For this reason they are preferred in patients with an increased risk of endocarditis. However, when their battery life is over, they cannot be removed. In this case a second leadless pacemaker or even a traditional cable pacemaker can be implanted.
