AORTIC STENOSIS
AORTIC STENOSIS
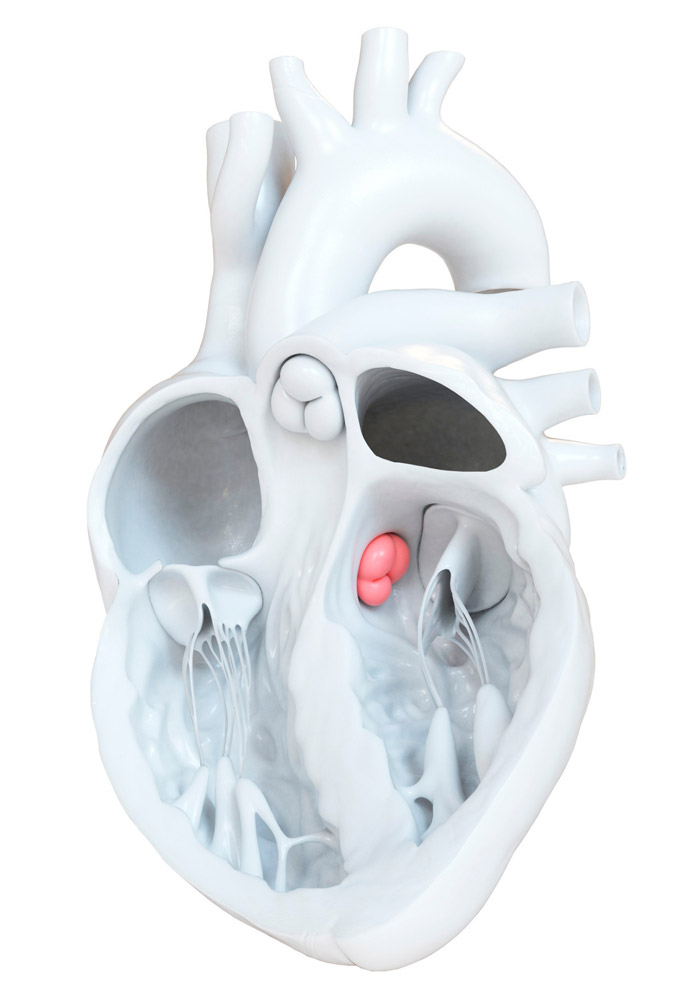
Aortic Valve connects the left ventricle with the ascending aorta, i.e. the central artery of the human body. Normally aortic orifice has an area of 3-4 cm2. When the area of the orifice is smaller then this is called aortic valve stenosis or simply aortic stenosis. In particular, when the area of the orifice is less than 1 cm2, this refers to severe aortic stenosis, which is usually accompanied by symptoms.
Aortic stenosis is one of the most common valvular diseases in the western world. In most of the times it is a degenerative valvular disease (that is, it occurs with growing age), it may be related with bicuspid aortic valve, while in the historically its leading cause was rheumatic fever.
The natural course of aortic stenosis is usually long and “silent”. Clinical presentation may include angina, syncope, and / or heart failure. Symptoms usually appear in the 7thor 8th decade of life (or in the 4-5th if it is related to a bicuspid aortic valve). Moderate aortic stenosis is estimated to aggravate into severe in 50% of patients within 5 years.
Symptoms onset is crucial, as the patient’s life-expectancy is reduced dramatically, if left untreated. Historical data estimate the life-expectancy of symptomatic severe aortic stenosis to 2-5 years, if treated under medications alone. However, if the valve is replaced then the patient’s estimated prognosis (life-expectancy) returns approximately to the previous levels, as if there were no aortic stenosis. The patient is diagnosed and monitored by echocardiography. In some cases, for a final diagnosis and grading of the severity a stress-echocardiogram may be required.
Additionally there are some cases in which the decision to proceed with aortic valve replacement is made, even if in the absence of symptoms. This occurs when severe aortic valve stenosis has been diagnosed with a) concomitant loss of left ventricular function or b) when significant findings occur during stress-echo (symptoms or drop in blood pressure).
Aortic valve replacement is traditionally performed surgically by a heart surgeon. The prosthetic valve is replaced by a mechanical valve (typically in patients younger than 60-65 years), or a bioprosthetis (in older patients). Bioprosthetic valves are constructed of porcine or bovine pericardium, but have a shorter lifespan than mechanical ones. On the other hand, the disadvantage of mechanical valves is the need for lifelong administration of anticoagulants.
In addition to the classic, surgical replacement of the aortic valve, transcatheter implantation by invasive cardiologists is possible. This method is called transcatheter implantation (replacement) of aortic valve – TAVI or TAVR (see related article). TAVI was initially introduced in clinical practiveonly for patients who were considered inoperable or of very high intraoperative risk. Recent data from large clinical trials are gradually expanding the range of patients who may be treated with TAVI.
