HYPETROPHIC CARDIOMYOPATHY
HYPETROPHIC CARDIOMYOPATHY
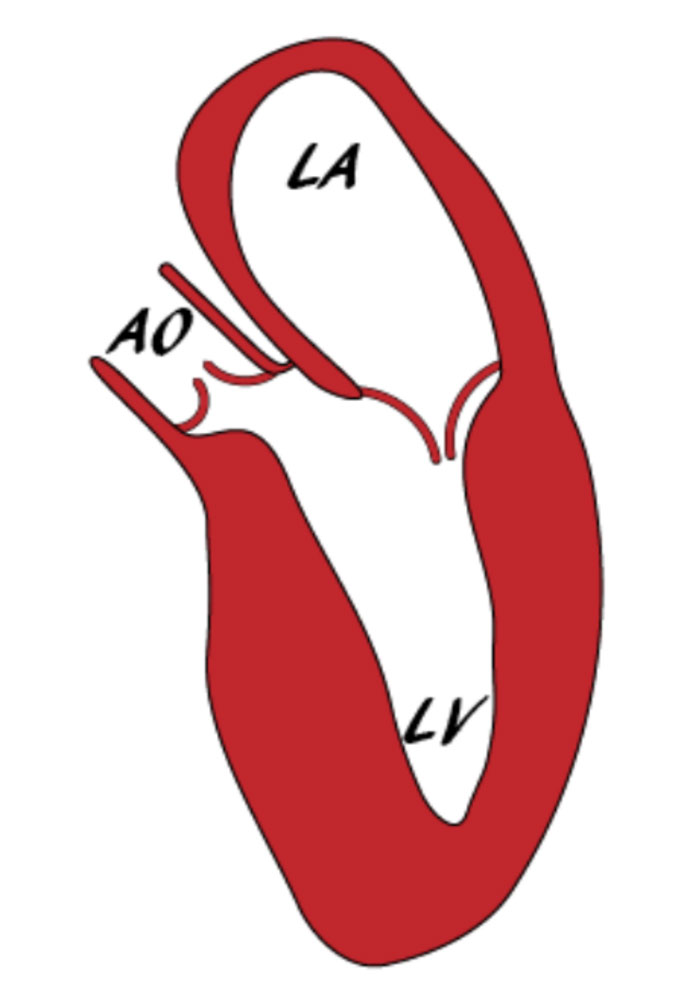
Hypertrophic cardiomyopathy is defined as an increase in the thickness of the walls of the left ventricle which can not be attributed to its loading conditions. It is a disease of cardiac sarcomere and is characterized by hypertrophy and disorganization of the cellular architecture.
Hypertrophic cardiomyopathy is hereditary – it is usually transmitted by an autosomal dominant type, but there are also cases of recessive heredity or even sex-linked disease (eg Anderson-Fabry disease).
Hypertrophic cardiomyopathy is the most common cause of sudden death in the young (<30 years old). The absolute annual risk is estimated to be approximately 1%. The majority of patients who suffer from sudden cardiac death in the context of hypertrophic cardiomyopathy were previously asymptomatic.
Findings in hypertrophic cardiomyopathy, beyond an increase in left ventricular wall thickness, include electrocardiographic disorders, disorders of the mitral apparatus, disorders of the coronary microcirculation as well as fibrosis of the myocardium with concomitant cardiac architecture disarray.
The disease may be asymptomatic for long. Symptoms usually present when left ventricular outflow obstruction occurs or worsens. Symptoms may include heart failure (fatigue, shortness of breath, etc.), myocardial ischemia (eg angina), seizures or pre-seizures, or sudden cardiac death.
The treatment of hypertrophic cardiomyopathy aims at:
- (a) the remission of symptoms; and
- (b) to prevent sudden death.
Patients should avoid dehydration, alcohol overdose and competitive sports. Treatment includes medication (usually non-vasodilating β-blockers) while cases of severe obstruction of the left ventricular outflow tract may require partial surgical resection of the interventricular septum or – if the surgical risk is high – invasive ablation utilizing an alcohol solution.
Sudden cardiac death is preventedby implantaion of a defibrillator. The decision to implant or not a defibrillator is made on the basis of the estimated risk of sudden cardiac death via special scores (which take into account left ventricular wall thickness, age, left ventricular outflow pressure gradient, non-persistent ventricular tachycardia, left atrial diameter, family history of sudden cardiac death and unexplained syncope). If the risk is estimated to be over 4% (especially over 6%) then defibrillator implantation is recommended. If it is below 4% with the presence of an additional risk factor the decision is individualized. If no additional risk factors exist, current instructions advise against implantation of a defibrillator.
It is easily understood that some of the variables taken into account in the assessment sudden death risk are dynamic. Follow-up of these patients should be close utilizing both echocardiography and holter rhtyhm monitoring, usually on an annual basis if the patient is stable and / or more frequently if deemed so.
Current guidelines (2014, European Society of Cardiology) recommend against the administration of chemoprophylaxis (preventive antibiotic therapy) as a routine in dental procedures.
First-degree relatives of patients with hypertrophic cardiomyopathy should undergo clinical and in the laboratory (electrocardiogram, echocardiogram) evaluation with a follow-up every 2-5 years. Children are screened starting at the age of ten (every 1-2 years until the age of 20, then every 2-5 years). Genetic testing, if required, is conducted in specialized centers and may modify follow-up intervals.
